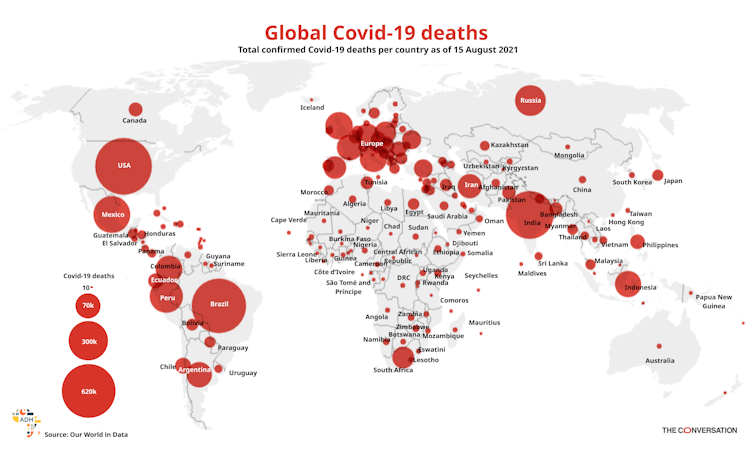
RESEARCH. There’s been an increase in COVID-19 deaths across Africa since mid-July 2021. But the impact of the pandemic in sub-Saharan Africa remains markedly lower compared to the Americas, Europe and Asia. In this article, a group of researchers offers some explanations.
The reasons for this are not yet clear. Several factors have been suggested as potentially influencing the low burden of COVID-19 illness. These include age demographics, lack of long-term care facilities, potential cross-protection from previous exposure to circulating coronaviruses, limitations of SARS-CoV-2 testing which may have resulted in an undercounting of deaths, and effective government public health responses.
In a recent paper our team of public health researchers, led by health analyst Janica Adams, examined these possible explanations by reviewing the scientific literature. The aim was to help guide public health decision making to contain COVID-19.
A number of hypotheses emerged from the literature review. In this article we explore the most common ones. More research is needed to better understand how these factors contribute to the lower burden of COVID-19 disease in the African context.
The young age demographic of sub-Saharan Africa
Age has been observed as a significant risk factor for severe COVID-19 illness. Most deaths occur in those aged 65 or older. The median age in North and South America, Europe and Asia ranges from 32 to 42.5 years. The age demographic structure of sub-Saharan Africa is much younger – the median age is 18.
The stark difference in age demographics can be demonstrated by comparing Canada and Uganda, which are similar in population size. In Canada, the median age is 41.1. Around 18% of the population is 65 or older. In contrast, the median age of Uganda is 16.7. Only 2% of the population is 65 or older. Canada has recorded nearly 1.5 million COVID-19 cases and 27,000 deaths compared to fewer than 100,000 cases and 3,000 deaths in Uganda. COVID-19 has a significant impact on older people. Countries with larger proportions of older people are more likely to be hardest hit.
Lack of long-term care facilities
Most elderly people in sub-Saharan Africa don’t live in long-term care facilities. These facilities pose significant risks for infectious diseases. COVID-19 has substantially affected those living in long-term care facilities. During the first wave of the pandemic, about 81% of deaths in Canada occurred in those facilities.
In sub-Saharan Africa, provision of care is mostly left to families. This limits the number of formal caregivers and thus reduces the chance of transmission. An exception to this is South Africa, which has an established long-term care sector. South Africa was the worst affected country in sub-Saharan Africa. And 33% of COVID-19 outbreaks in South Africa occurred in long-term care facilities during the first wave.
Potential cross-protection from local circulating coronaviruses
It’s been suggested that prior exposure to circulating coronaviruses could reduce the severity of COVID-19 illness if people have developed antibodies. A previous study demonstrated that prior exposure to endemic coronaviruses resulted in lower chance of death and lower disease severity compared to those who were not previously exposed. Human-bat interactions are common in some rural areas of Africa.
Limitations of SARS-CoV-2 testing
There are concerns that the limited SARS-CoV-2 testing may have resulted in an undercounting of COVID-19-related deaths in sub-Saharan Africa. Insufficient data collection may mean we don’t really know the incidence and prevalence of COVID-19. Though varying across sub-Saharan Africa, testing levels have been low compared to other areas of the world.
Effective government public health response
The rapid response of several African governments and health organisations may have played a significant role. At the beginning of the pandemic, several measures were taken: screening, establishment of the Africa Task Force for Novel Coronavirus, suspension of flights from China and closure of borders in 40 African nations. New programmes also promote sharing of COVID-19 information across sub-Saharan Africa.
In contrast to high-income countries which focus on non-communicable diseases, health organisations in sub-Saharan Africa focus on infectious diseases. The formation of national public health institutions has been key in curbing infectious diseases in Africa through disease surveillance, diagnostics and rapid response to outbreaks.
But stringent lockdowns have taken a serious economic and societal toll across sub-Saharan Africa. Lockdowns resulted in increased food insecurity, teenage pregnancy, gender-based violence, and disruptions in treatment of malaria, TB and HIV. Africa’s 54 nations are not all the same, and local responses should be tailored to the health, social and economic realities in specific countries.
South Africa: the outlier
In contrast to the rest of sub-Saharan Africa, South Africa has experienced higher proportions of COVID-related hospitalisations and deaths. South Africa has a remarkably higher median age and a long-term care sector. In addition, the higher rates of HIV and TB in South Africa have been associated with higher COVID-19 death rates. The prevalence of noncommunicable disease in South Africa is higher than in other regions, which may contribute to the higher burden of COVID-19 disease. South Africa also has better diagnostic capabilities and healthcare documentation than other sub-Saharan African countries. This may contribute to higher reporting rates.
Recommendations
We believe that the low median age and a small percentage of vulnerable elderly contribute significantly to sub-Saharan Africa’s lower COVID-19 death rates.
Based on our research, we propose several policy prescriptions to help improve health practice.
Lockdowns lead to severe health consequences for the young and the poor in the African context. Therefore, reduced emphasis on lockdowns should be considered.
Better communication with the public is required to help curb COVID-19.
Governments should find adequate financial support for vulnerable sectors, possibly from external agencies.
Governments and health agencies should ensure that medical infrastructure is available in the case of a severe outbreak, as seen with the oxygen shortage in India.
International efforts should prioritise developing vaccines that are effective against virus variants of concern and ensuring equitable access to such vaccines.
The emergence of variants of concern with increased potential for transmission and more severe disease in the younger population could make Africa more susceptible to a severe COVID-19 epidemic. These variants need to be monitored through molecular epidemiologic surveillance. And further studies are needed to better understand potential mechanisms of severe disease in the African context.
Alex Ezeh
Dornsife Endowed Professor of Global Health, Drexel University
Michael Silverman
Chair of Infectious Diseases, Schulich School of Medicine & Dentistry, Western University,
Saverio Stranges
Professor & Chair of Epidemiology, Western University
This article is republished from The Conversation under a Creative Commons license. Read the original article here.
Listen also to


